Common Pediatric Visits
Matthew Rensberry, MD, MBA
April 28, 2021
Common Pediatric Encounters
- Routine child health exam (22.9%)
- Otitis media (6.6%)
- Acute upper respiratory infection (4.6%)
- Acute pharyngitis (3.4%)
- Attention-deficit/hyperactivity disorder (3.2%)
- Asthma (2.8%)
- Chronic sinusitis (2.4%)
- Immunization visits (2.3%)
- Streptococcal sore throat (1.9%)
- Allergic rhinitis (1.9%)
Routine Well-Child Health Exam
- History
- Physical Examination
- Screening
- Immunizations
- Anticipatory Guidance
History
- Birth history
- Prior screenings
- Diet
- Sleep
- Dental care
- Medical, Surgical, Family, and Social histories
Physical Examination
- Head-to-toe examination
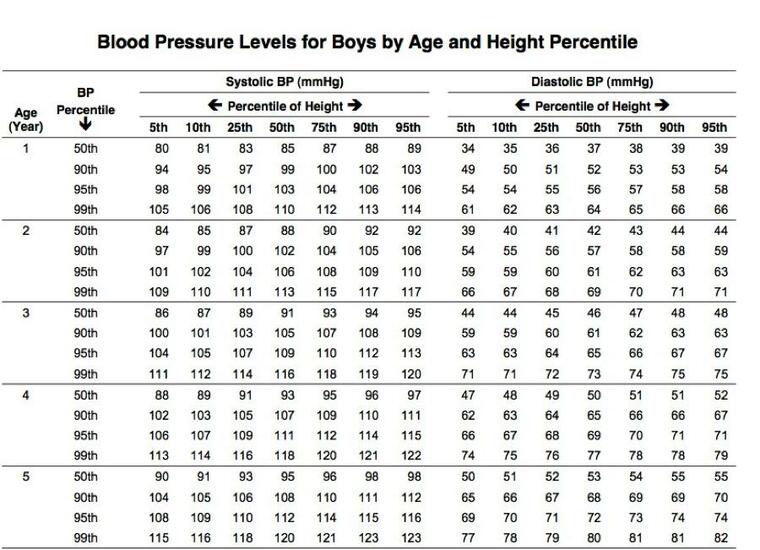
- Blood pressure
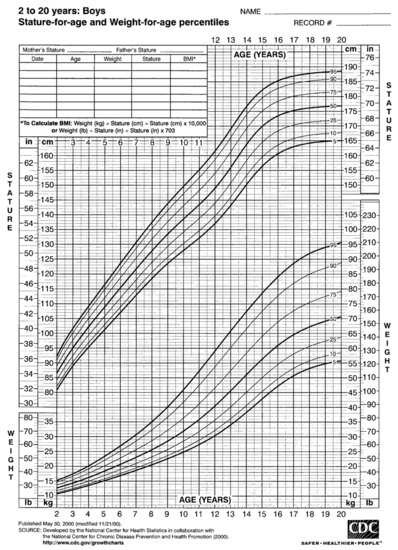
- Review of growth
Blood Pressure Chart Example
Pediatric Growth Chart Example
Screening
- Developmental surveillance (9, 18, and 30 mo of age)
- CDC App: Milestones
- Postpartum depression screening
- Mothers of infants up to six months of age
- Psychosocial
- Vision
- Iron Deficiency (slightly controversial)
- Lead for high risk
Immunizations
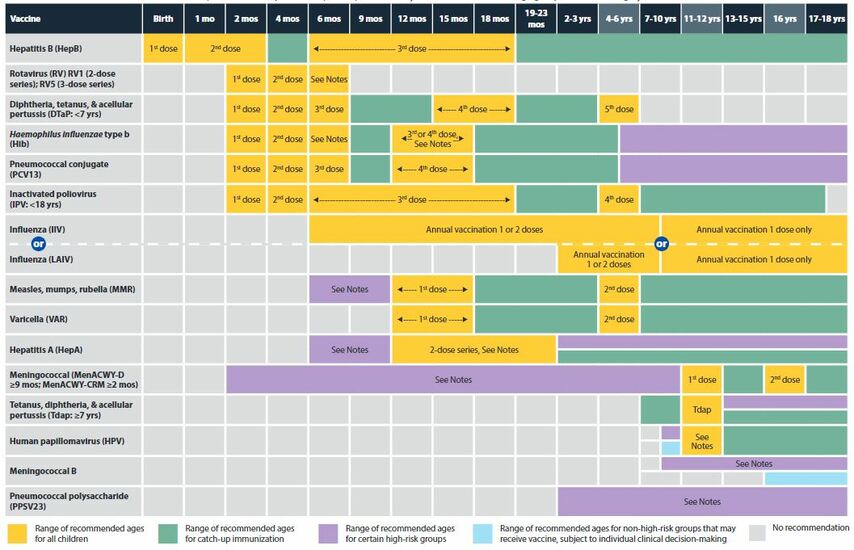
Immunizations
- Reviewed and updated as appropriate.
- Typically given at:
- 2 month, 4 month, 6 month, 12 month, 15 month, and 18 month visits
- 4 yo and 6 yo visits
- Annually during influenza season
- CDC App: Vaccine Schedules
- AAFP/STFM App: Shots Immunizations
Anticipatory Guidance
- Provide age-appropriate guidance:
- Breastfeeding
- Car seats
- Dental health
- Early introduction of highly allergenic foods (peanut-based foods and eggs), before one year
- Juice and sugar-sweetened beverages
- Physical Activity (Play time)
- Screen Time
Otitis Media
Otitis media
The most common pathogens:
- Non-typeable H. influenzae
- S. pneumoniae
- M. catarrhalis
- Viruses
- Group B streptococcus, gram-negative enteric bacteria, and Chlamydia trachomatis
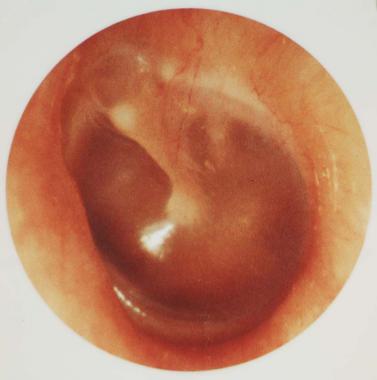
Diagnosis
Diagnosis requires:
- Acute onset of symptoms
- Presence of middle ear effusion
- Signs and symptoms of middle ear inflammation
Diagnosis
Diagnosis of AOM is not made due to:
- Acute otitis externa
- Mild bulging of the TM and recent (less than 48 hours) onset of ear pain
- Intense erythema of the TM
Management
- Antibiotic therapy should be considered for children 6-35 months of age with AOM (LOE B)
- First line: Amoxicillin, 80-90 mg/Kg/d, in two divided doses
- Second line (or if vomiting): Ceftriaxone (Rocephin)
- Antibiotic therapy should be prescribed:
- For Bilateral AOM in 6 - 23 month old without severe signs or symptoms
- For AOM (bilateral or unilateral) in children >6 months with severe signs or symptoms
Management
- Antibiotic Observation option:
- Children 6-23 mo with nonsevere unilateral AOM
- Children >24mo with nonsevere AOM (either unilateral or bilateral)
- Assess pain in children diagnosed with AOM.
- Tympanostomy tubes may be offered for recurrent AOM:
- 3 episodes in 6 months
- 5 episodes in 18 months
Medication Calculation Practice
John is a 12 month old male who weighs 9 Kg. You diagnose him with AOM. What are your instructions for his antibiotic medication?
(Goal dose: 80 to 90 mg/Kg/day divided twice a day)
Medication Calculation
- 80 mg/Kg/day divided in 2 = 80 mg * 9 Kg / 2 => 720 mg/day
- Divided twice a day: 720 mg / 2 = 360 mg/dose
- 90 mg/Kg/day divided in 2 = 90 mg * 9 Kg /2 => 810 mg/day
- Divided twice a day: 810 mg / 2 = 405 mg/dose
Medication Calculation
Amoxicillin availability:
- 125 mg / 5 mL
- 200 mg / 5 mL
- 250 mg / 5 mL
- 400 mg / 5 mL
You choose to order 10 days of 400 mg / 5 mL at 400 mg twice a day = 100 mL
Prognosis
- AOM typically resolves without antibiotic therapy in children
- Children with AOM should be re-evaluated in 3 months
Acute Upper Respiratory Infection
Characterized by:
- Cough
- Nasal congestion
- Rhinorrhea
- Sneezing
- Sore throat
Management
- Symptomatic treatment
- Antibiotics are not recommended
- Antibiotics should not be prescribed for acute laryngitis. (LOE A)
- Don't use albuterol in children with bronchiolitis
Acute Bacterial Sinusitis (AAP Guidelines)
- Diagnosed in older children with an acute upper respiratory infection that persists:
- Over 10 days of nasal discharge or daytime cough
- Worsening condition after improving at first
- Severe (concomitant fever of at least 102.2˚F [39˚C] and purulent nasal discharge for >3 days)
Bacterial Sinusitis Management
- Antibiotics should be prescribed in children with:
- Severe
- Worsening
- or Persistent acute bacterial sinusitis
- First-line: Amoxicillin alone or in combination with clavulanate
Acute Pharyngitis
- Approximately 70% of children with pharyngitis have viral infections
- Manage symptomatically
- When bacterial, the most common pathogen is: Group A beta-hemolytic streptococcus
Acute Pharyngitis
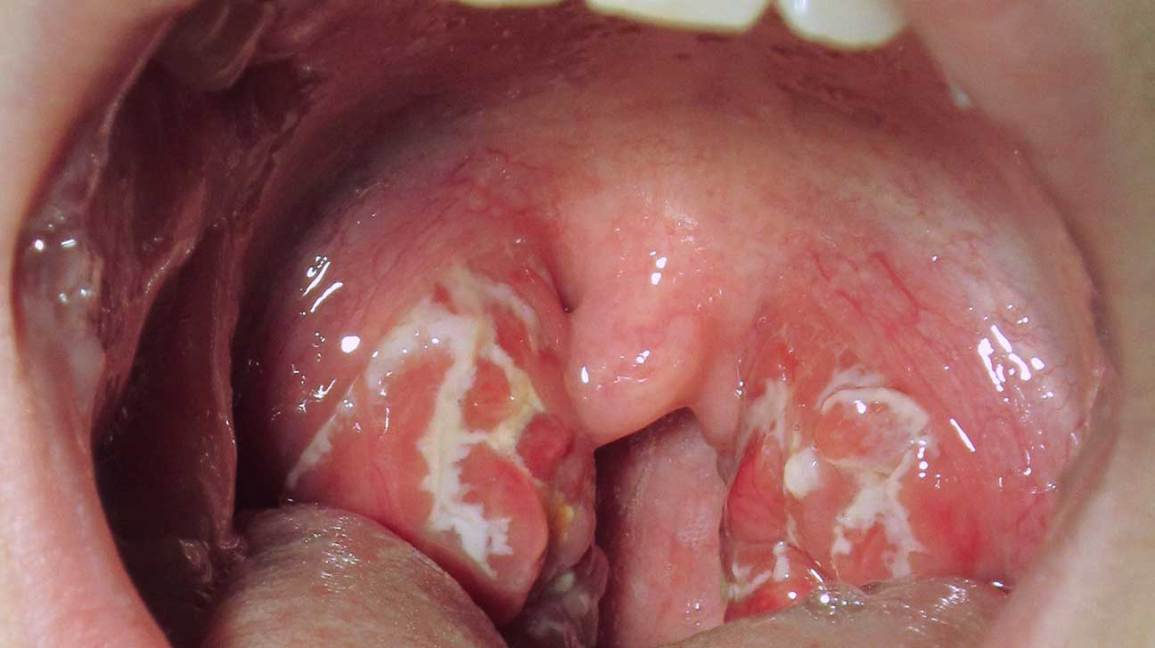
Assess risk for Bacterial Pharyngitis
| Absence of cough | 1 |
| Age 3 to 14 years | 1 |
| Anterior cervical lymphadenopathy | 1 |
| Fever | 1 |
| Tonsillar erythema or exudates | 1 |
Centor Scoring
- 0 to 1: No further diagnostic testing or treatment indicated
- 2 to 3: Perform streptococcal rapid antigen detection testing - if positive, treatment is indicated
- 4: Antibiotic therapy is recommended
Streptococcal pharyngitis
Penicillin should be used in patients with streptococcal pharyngitis (LOE B)
- Appropriate antibiotic treatment:
- Decreases the risk of rheumatic fever
- Decreases communicability
- Alleviate symptoms (by ~1 day)
- Antibiotic treatment:
- Does not prevent glomerulonephritis
- Inconsistent results in the prevention of peritonsillar abscess
Attention-Deficit/Hyperactivity Disorder (ADHD)
- Most common behavioral disorder in children
- Many coexisting conditions
- These are At-risk individuals!
Diagnosis
- Cannot be reliably diagnosed in children <4 years of age
- NICHQ Vanderbilt Assessment Scales (Ages 6 to 12)
Management (Goal)
Goal of ADHD treatment:
- Improve symptoms
- Optimize functional performance
- Remove behavioral obstacles
Management (Behavioral Therapy)
- Behavioral therapy should be the primary treatment for ADHD in children <6 years of age (LOE B)
- Effective behavioral therapies:
- Parent training
- Classroom management
- Peer interventions
Management (Medications)
- Medications are recommended as first-line therapy for older children. (LOE B)
- Psychostimulants are most effective for the treatment of core ADHD symptoms and have generally acceptable adverse effect profiles. (LOE B)
- Examples: methylphenidate and dextroamphetamine
- Atomoxetine, guanfacine, and clonidine, are less effective than the psychostimulants
- Psychostimulants are most effective for the treatment of core ADHD symptoms and have generally acceptable adverse effect profiles. (LOE B)
Management (Encounters)
- Monthly visits initially
- Record at follow-up visits:
- Height
- Weight
- Heart rate and blood pressure
- Symptoms
- Mood
- Treatment adherence
Asthma
Acute childhood asthma is a common clinical emergency!
Asthma
- Chronic inflammatory disease of the airways:
- Episodic wheezing
- Reversible airway obstruction
- Acute exacerbations:
- Tachypnea
- Increased work of breathing
- Tachycardia
- Reduced oxygen saturation levels
Severity (Moderate Acute Asthma)
- Oxygen saturation level: 92%-95%
- Pulse: 100-125bpm (>5yo) or 120-140bpm (2-5yo)
- Respiratory rate: 20-30bpm (>5yo) or 30-40bpm (2-5yo)
- Some use of accessory muscles (>5yo) or some chest wall recession (2-5yo)
- Talking in short phrases.
Severity (Severe Acute Asthma)
- Oxygen saturation level: <92%
- Pulse: >125bpm (>5 yo) or >140bpm (2- 5yo)
- Respiratory rate: >30bpm (>5yo) or >40bpm (2-5yo)
- Use of accessory muscles (>5yo) or obvious chest wall recession (2-5yo)
- Inability to complete sentences in one breath (the child speaks 1 or 2 words)
- Too breathless to feed
Triggers
- Viral infection (Predominant cause, detected in 80%-85% of cases)
- Exercise
- Allergen exposure (inhaled or ingested)
- Cold weather
- Poor air quality
EBM Medication Management
Beneficial:
- Beta 2 agonists (high-dose inhaled)
- Corticosteroids (high-dose inhaled)
- Corticosteroids (systemic)
- Ipratropium bromide (inhaled)
- Magnesium sulfate (intravenous)
- Oxygen
- Salbutamol (intravenous)
Likely to be beneficial:
- Theophylline or aminophylline (intravenous)
Asthma Management
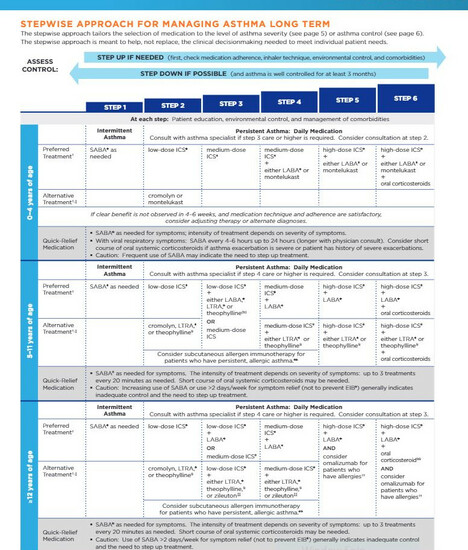
Admission Risk Factors
Risk factors for asthma admissions:
- Not having or not adhering to a written crisis management plan (Asthma Action Plan)
- Inappropriate preventive treatment
- Poor compliance
- Delay of more than 24 hours in seeking advice
Not all wheezing is asthma…
- Children <5 yo with lower respiratory tract infection or foreign body aspiration can present with asthma like symptoms
Chronic Rhinosinusitis
- Occurs in 1% to 5% of the U.S. population
- An inflammatory disease of the paranasal sinuses
Diagnosis
- Chronic rhinosinusitis has at least 2/4 cardinal symptoms for >3 mo and objective evidence:
- Nasal obstruction (81% to 95% of patients)
- Facial pain/pressure (70% to 85%)
- Nasal drainage (51% to 83%)
- Hyposmia/anosmia (61% to 69%)
- Objective evidence:
- Physical examination (anterior rhinoscopy, endoscopy)
- Radiography (preferably sinus computed tomography)
Goals of Therapy
- To enhancing mucociliary clearance
- Improving sinus drainage/outflow
- Eradicating local infection and inflammation
- Improve access for topical medications
Treatment
- First-line treatment is nasal saline irrigation and intranasal corticosteroid sprays
- Daily low-pressure/high-volume (240mL) saline irrigations (NNT=2)
- There may be a role for antibiotics in patients with evidence of an active, superimposed acute sinus infection
- If medical management fails, endoscopic sinus surgery may be effective
- Patients not responding to first-line medical therapy should be referred to an otolaryngologist
Allergic Rhinitis
- Symptoms:
- Rhinorrhea
- Sneezing
- Nasal congestion, obstruction, and pruritus
Symptom Classification
- Temporal pattern
- Seasonal
- Perennial
- Episodic
- Frequency
- Intermittent (>4d/wk)
- Persistent (>4wks/yr)
- Severity
- Mild
- Severe
Management (Things that work)
(These Work!)
- Avoid known allergens
- Intranasal corticosteroids (most effective treatment)
- Second-line therapies:
- Antihistamines
- Leukotriene receptor antagonists
- Nonpharmacologic therapies (nasal irrigation)
Management (Things that don't work)
Things we have recommended that lack evidence of effectiveness (LOE A/B):
- Breastfeeding
- Air filtration systems
- Delayed exposure to solid foods in infancy or to pets in childhood
- Mite-proof impermeable mattresses and pillow covers
Other General Stuff
General Parenting Strategies
- Catch them being good
- Let them help you
- Establish home routines
- Monitor your children
- Hand out discipline in a consistent manner
- Save long talks and lectures for good behavior
- Show sympathy when you discipline
- Be a good role model
- Be a parent, not a martyr
- As a parent, understand that you are also a teacher
- Monitor your children's use of electronic media
Some final recommendations…
- Do:
- Provide access to long-acting reversible contraception for adolescents
- Promote childhood literacy development by providing free, age-appropriate books in clinical settings
- Don't:
- Don't perform computed tomography of the head for children with minor head trauma
Connect with Me
- Website: anchor-dpc.com
- Facebook: MatthewRensberryMD
- LinkedIn: Matthew-Rensberry-MD
- Twitter: @RensberryMD
- Email: Dr.Rensberry@anchor-dpc.com